Our 3C’s To Combat The Big C

Clarity
The value of performing mammography (MMG) to detect and diagnose breast cancer has been validated by a number of clinical trials.1-3 However, mammographic detection of breast cancer in dense breasts presents a challenge. Fibro-glandular tissue in dense breasts can mask cancer such that sensitivity is substantially lower than for breasts that contain predominantly fatty tissue or have scattered density.4-5
To be Clear is to be Enlightened
Because of the decreased sensitivity of mammography (MMG) to detect cancer in dense breasts, supplemental imaging must be done to prevent delayed diagnosis. The sooner cancer can be identified, the smaller and earlier stage the cancer is and, consequently, better patient outcomes can be achieved with less traumatic treatment options. Radiologists have relied on supplemental imaging modalities such as ultrasound (US), digital breast tomosynthesis (DBT, also called “3D-mammography”), contrast-enhanced spectral mammography (CESM), and magnetic resonance imaging (MRI). Each offers incrementally better breast cancer detection in dense breasts than mammography alone. However, Eve Clear Scan™, using molecular breast imaging (MBI) technology, is superior to all of these methodologies.
An MBI examination employs an intravenous (IV) injection of a gamma-emitting tracer, Tc-sestamibi. Image acquisition can begin nearly immediately after injection while the breast is gently immobilized (not painful: about 1/3 of the force used in mammography). Cancer cells avidly take up the tracer molecules and the emitted gamma rays are detected by a specialized gamma camera.6
SmartBreast offers two types of gamma camera systems for image acquisition:

Eve Clear Scan™ model e750 uses solid state cadmium-zinc-telluride (CZT) technology and compact dual detector design to allow for up- close breast imaging to the chest wall. The result is improved lesion detection, intrinsic resolution, spatial resolution, sensitivity, and degradation-free image uniformity.

Eve Clear Scan™ model e680 uses a compact sodium iodide (NaI) single detector design, optimized for breast specific gamma imaging (BSGI). It is a portable system, which enables the user to move and position the machine in a desired location.
The strikingly distinctive images produced by MBI provide clear visibility of the cancer in contrast to the generally unhelpful mammographic images in dense breasts.
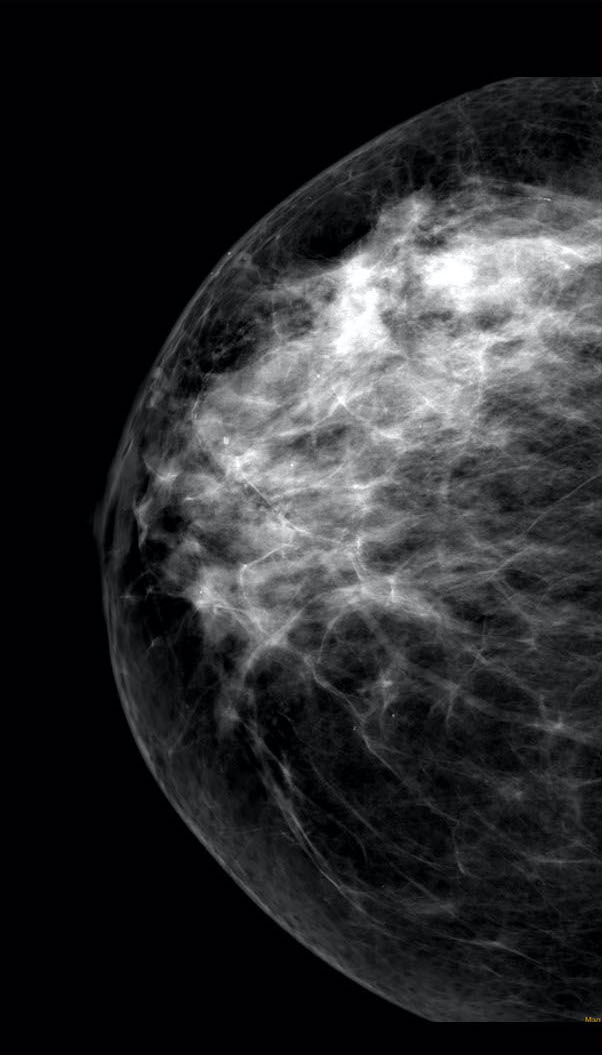
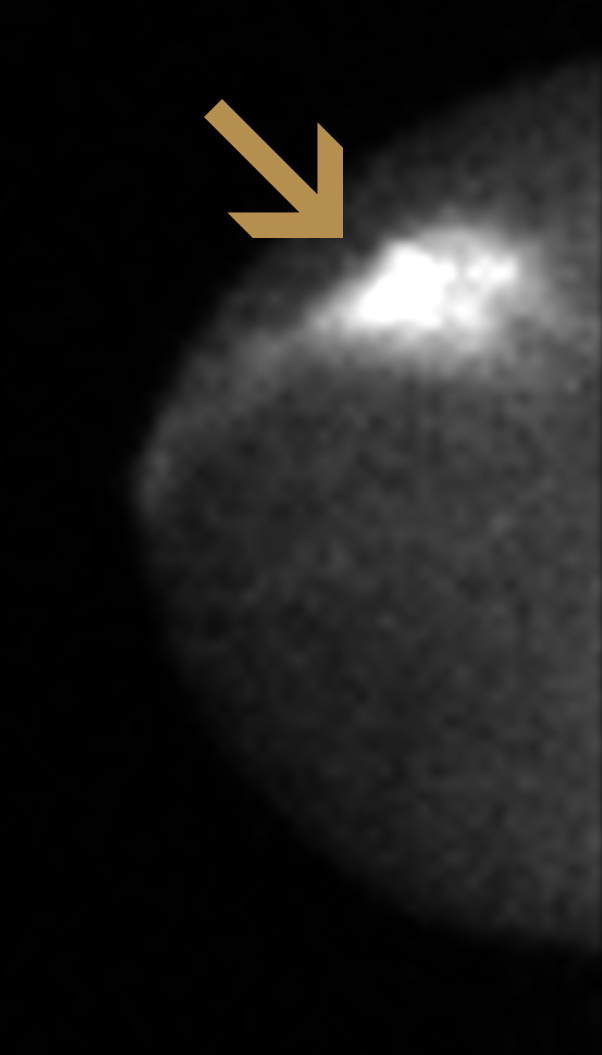
Example Case: 46-year-old woman with family history of breast cancer (mother)
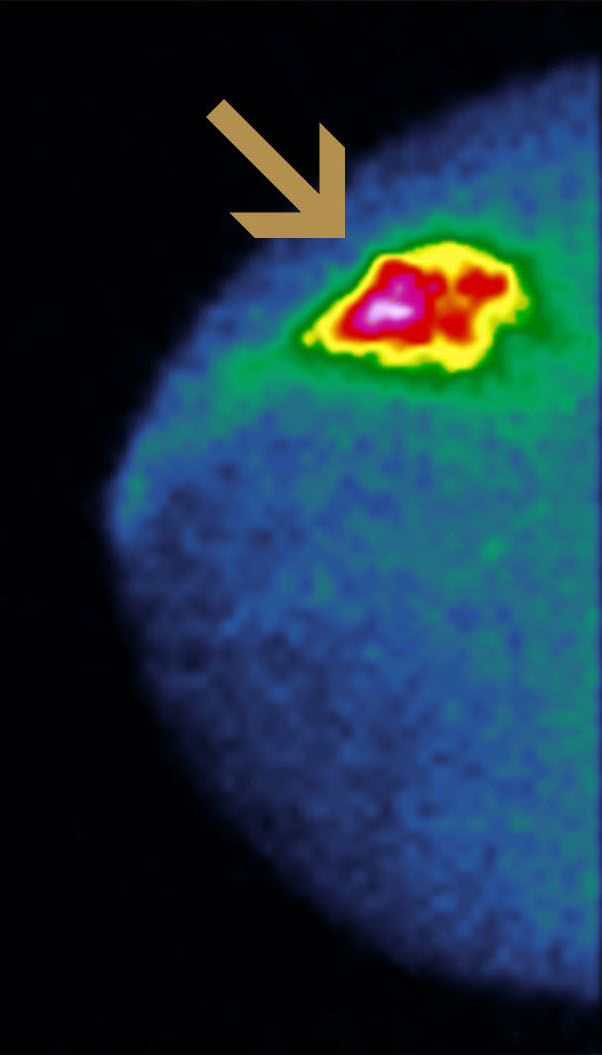
(COLORED)
Right cranio-caudal (CC) mammographic projection (far left) shows a heterogeneously dense breast that was interpreted as normal. Right CC MBI image (middle) shows intense tracer uptake in 3-cm cancer mass (arrow). Color mapping of same MBI image (right) shows distinctive tracer uptake. Biopsy was performed under ultrasound guidance, identifying invasive cancer.
Our Vision is Your Power
The many clinical uses of MBI are becoming better established as more published data have become available. The American College of Radiology in 2017 issued “Practice Parameters for the Performance of MBI Using a Dedicated Gamma Camera” and cited the potential indications for using MBI:7
- Extent of disease/preoperative staging in newly diagnosed breast cancer
- Evaluation of response to neoadjuvant chemotherapy
- Detection of local breast cancer recurrence
- Evaluation for primary breast cancer in women with metastases or metastatic axillary lymphadenopathy of unknown primary
- Breast cancer screening
- MBI as adjunct to conventional breast imaging for problem solving in indeterminate cases
The diagnostic yield of MBI has been compared to CESM and MRI in 99 women with biopsy-proven newly diagnosed cancers (65% had dense breasts). All three (3) modalities have shown similar sensitivity to visualize the known cancers, but CESM and MBI have higher specifity (ability to predict malignancy) for additional cancers detected compared with MRI.8
Furthermore, MBI is a better imaging method over MRI in the following situations:
- If you have any metal within your body, such as from a cochlear implant, clip in the brain, or cardiac implantable electronic devices (e.g., pacemaker, cardioverter defibrillator)
- If you have claustrophobia
- If you are overweight and find it difficult to lay on your stomach for up to an hour
- If you have severe allergies to medications or contrast agents
- If you have poor kidney function
References
1 Shapiro S, Strax P, Venet L. “Periodic breast cancer screening in reducing mortality from breast cancer”. JAMA 1971; 215(11): 1777–1785.
2 Tabar L, Yen MF, Vitak B, Chen HH, Smith RA, Duffy SW. “Mammography service screening and mortality in breast cancer patients: 20-year follow-up before and after introduction of screening”. Lancet 2003; 361(9367): 1405–1410.
3 Jonsson H, Nyström L, Törnberg S, Lenner P. “Service screening with mammography of women aged 50-69 years in Sweden: effects on mortality from breast cancer”. J Med Screen 2001;8(3): 152–160.
4 Boyd NF, Guo H, Martin LJ, et al. “Mammographic density and the risk and detection of breast cancer”. N Engl J Med 2007; 356(3): 227–236.
5 Sickles EA. “The use of breast imaging to screen women at high risk for cancer”. Radiol Clin North Am 2010; 48(5): 859–878.
6 Hruska CB, Weinmann AL, Tello Skjerseth CM, et al. “Proof of concept for low-dose molecular breast imaging with a dual-head CZT gamma camera. Part 2. Evaluation in patients”. Med Phys 2012; 39: 3476–3483
7 American College of Radiology Council. “ACR Practice Parameters for the Performance of Molecular Breast Imaging (MBI) Using a Dedicated Gamma Camera. Oct 2017. Res 38.
8 Sumkin JH, Berg WA, et.al. “Diagnostic performance of MRI, molecular breast imaging, and contrast-enhanced mammography in women with newly diagnosed breast cancer”. Radiology 2019; 293:531–540
